The statistics about stress have been alarming for awhile – and yet data shows the impact is only growing. Looking at the latest and historical numbers can help us understand how stress is shaping everyday life in the U.S. and what factors are driving it.
- More than a quarter (27%) of American adults report being so stressed, they cannot function, according to a poll conducted by the American Psychological Association in 2022.
- In 2024, APA also reported as many as 70% of primary care visits were driven by patients’ psychological problems, such as anxiety, panic, depression, and stress.
Worry is widespread
As a nation, stress arises from many sources – rising inflation, looming work deadlines, and relationship struggles, to name a few.
But as of this writing, the future of the country remains the greatest concern, with an overwhelming 76% of Americans expressing worry about what lies ahead, according to recent data.
Top 3 most stressed U.S states
New Mexico, Nevada, and Louisiana top the list of most stressed states in the U.S. in 2025. WalletHub analyzed stress levels across all 50 states using 40 key metrics to help individuals identify the best places to live for a more relaxed lifestyle.
The analysis considered factors such as average weekly work hours, personal bankruptcy rates, and the percentage of adults who get sufficient sleep, providing a comprehensive look at stress distribution nationwide.
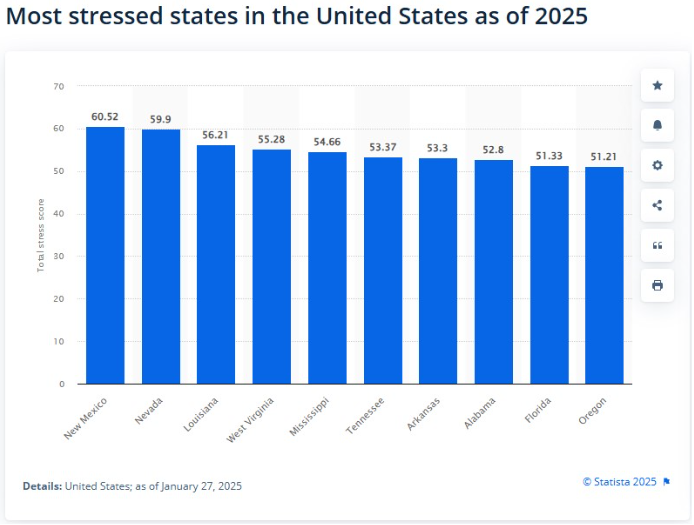
1. New Mexico
New Mexico ranks as the most stressed state in the U.S. due to high crime rates, the highest divorce rate, a large number of single-parent households, and significant financial struggles, including high poverty and low credit scores. These factors create significant daily challenges for residents.
2. Nevada
Nevada is the second-most stressed state in the U.S., driven by financial struggles like high unemployment, bankruptcy rates, and a low median credit score. Family stress is also common, with high rates of divorce and single-parent households. Health concerns, limited healthcare access, and low insurance coverage further add to residents’ challenges.
3.Louisiana
Louisiana is the third-most stressed state in the U.S., driven by high poverty, poor mental health rates, limited access to care, and low job security. With one of the highest unemployment rates and fewer psychologists per capita, many residents face significant barriers to well-being, including skipping medical care due to cost concerns.
Stress in the workplace: Then and now
The workplace continues to be a major source of stress, but the way we experience it has shifted over the past years.
Then (Historical context – roughly pre-2010s to early 2010s)
While comprehensive, regularly tracked statistics on workplace stress weren’t as prevalent in earlier decades as they are today, some key indicators emerged:
- General stress levels: In 2007, the American Psychological Association (APA) reported that Americans rated their stress level as 6.2 on a scale of 1 to 10. This provides a baseline for overall stress. (Pharmacytimes.com, 2015)
- Early recognition of work stress: Even decades ago, job stress was recognized as a major stressor for American adults and was noted to be escalating. Factors like high job demands and a lack of worker control were already identified as contributors to increased risk of cardiovascular disease. (The American Institute of Stress)
Now (Recent data – roughly 2010s to 2025)
The data strongly indicates a surge in workplace stress, with more widespread reporting and deeper understanding of its impacts.
- 83% of U.S. workers suffer from work-related stress. (BHHC Safety Center)
- 75% of employees report experiencing some form of low mood as of early 2025 (Modern Health Report via Business Wire)
- 76% of U.S. workers reported at least one symptom of a mental health condition (U.S. Surgeon General).
- 52% of employees are experiencing burnout. (NAMI.org)
- A majority of U.S. workers (54%) say job insecurity has a significant impact on their stress, often linked to government policy changes and economic uncertainty. (APA 2025 Work in America Survey)
- Technology and “always-on” culture (Calm’s 2024 Voice of the Workplace Report):
- 58% of employees agree they are always connected or available for work.
- 46% of employees often work outside working hours.
- One in three workers are often interrupted by their devices.
- 32% feel tired from being online for work.
- 45% of employees worrying that AI will take over their jobs, and 53% experiencing anxiousness due to the rapid pace of technology developments. (Microsoft.com)
- U.S businesses lose up to $300 billion yearly as a result of workplace stress. (The American Institute of Stress)
- Stress causes around one million workers to miss work every day. (BHHC Safety Center)
- Work-related stress causes 120,000 deaths and results in $190 billion in healthcare costs yearly. (BHHC Safety Center)
- 40% of job turnover is due to stress. (The American Institute of Stress)
Stress by demographics: Who feels it the most
Generally, younger adults in the U.S. tend to report higher levels of stress compared to older adults. This trend has been consistent across several years of data.
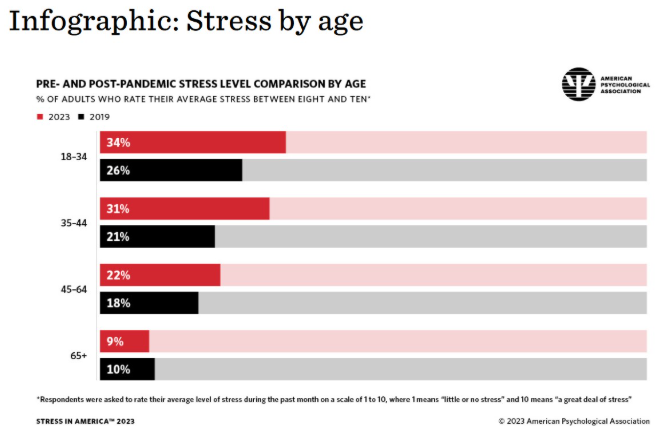
- Gen Z adults (18-29) and Younger Millennials (30s-early 40s) are particularly affected. In APA’s 2023 Stress in America survey, 18- to 34-year-olds reported an average stress level of 6 out of 10, compared with 3.4 among people ages 65 and older (American Psychological Association).
- Teenagers also report high stress levels (American Institute of Stress).
- On a 10-point scale, where adult stress averages 3.8, American teens rate their stress at 5.8.
- 75% of high school students and 50% of middle schoolers consistently feel stressed due to schoolwork.
- 70% of U.S. teens (ages 13-17) identify anxiety or depression as major issues among their peers.
- 37% of high school students reported their mental health was not good most or all of the time during the pandemic (Pew Research Center).
Key Stressors for younger age groups
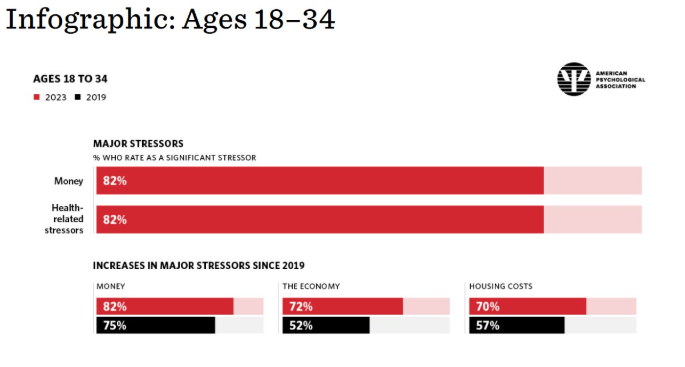
Younger adults and teens face stressors such as
- Financial woes: Especially for 20- and 30-somethings, 67% of 18- to 34-year-olds and 63% of 35- to 44-year-olds feel “consumed” by worries about money, compared to 13% of people 65 and older (American Psychological Association).
- Social isolation/connection: Younger adults (18-34) are more likely than older adults (50+) to say that social connection has the biggest impact on their mental health. 74% of those ages 18 to 34 and 70% of those ages 35 to 44 say it’s harder to connect with people today than in the past. (American Psychological Association)
- Current events and societal issues: Gen Z is more stressed about issues like mass shootings (75%), separation and deportation of immigrant families (57%), and sexual harassment and assault reports (53%) compared to adults overall (Biospace.com).
Gender disparities in stress data
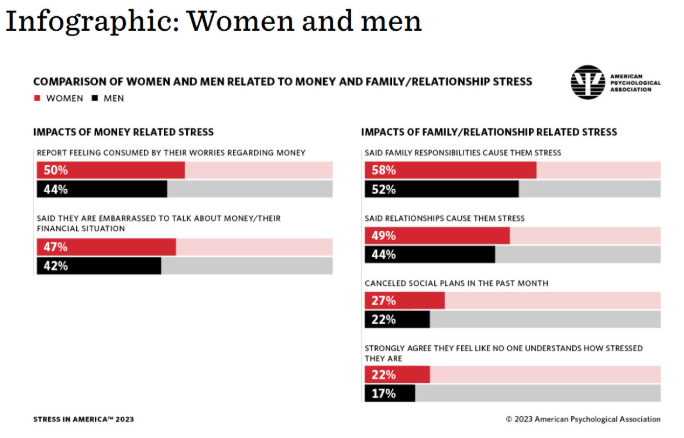
Women consistently report higher levels of stress than men.
- Average stress levels: In APA’s 2023 survey, women placed their stress levels at an average of 5.3 out of 10, while men reported an average of 4.8 out of 10 (Singlecare.com).
- Extreme stress: 23% of women reported their stress level at an 8, 9, or 10 on a 10-point scale, compared to 16% of men (2012 data, but this trend is consistent) (American Psychological Association).
- Increasing stress: More women say their stress levels have increased in the past five years (43% vs. 33% of men) and in the past year alone (38% vs. 32% of men) (2012 data, consistent trend) (American Psychological Association).
- Common stressors: Women are more likely than men to report stress about money, family responsibilities, and relationships (Singlecare.com).
- Wage gap and mental health: Women who earn less than their male peers are at greater risk for anxiety and depression. Among women whose income was lower than their male counterparts, the odds of major depression were nearly two-and-a-half times higher, and odds of anxiety were more than four times higher (Columbia.edu).
Ethnic and racial disparities in stress data
Racial and ethnic minority groups often experience unique stressors, including discrimination, which can lead to higher levels of stress and poorer mental health outcomes.
Discrimination as a stressor:
- In 2018, 46% of Black adults and 36% of Hispanic adults reported discrimination as a significant source of stress, compared with 14% of White adults (Biospace.com).
- 27% of adults overall cited discrimination as a substantial stressor in 2023. Black and Latino/a/e adults are more likely to experience discrimination and feel uncomfortable discussing it (Casatondemand.org).
Mental health conditions and stress:
- Hispanic/Latino adults reported a higher prevalence of psychosocial stress related to not having enough food or stable housing than did adults in other racial and ethnic groups during the COVID-19 pandemic (CDC.gov).
- Symptoms of current depression were reported 59% more frequently by Hispanic adults (40.3%) than by non-Hispanic White persons (25.3%)(CDC.gov).
- Estimates of self-reported suicidal thoughts/ideation among Hispanic persons (22.9%) were four times those among non-Hispanic Black persons (5.2%) and White persons (5.3%)(CDC.gov).
Social determinants of health:
Racial and ethnic minorities often face greater exposure to social determinants of health stressors, such as:
- Food insecurity: Black persons reported not having enough food three times more frequently, and Hispanic persons two times more frequently, than White persons (2019 data) (CDC.gov).
- Loss or reduced hours of employment: Multiracial individuals (1.48 times higher odds), Black/African American individuals (1.39 times higher odds), and Hispanic/Latino individuals (1.32 times higher odds) had a higher prevalence compared to White adults in 2022 (CDC.gov).
- Lack of social and emotional support: More prevalent in Asian (1.76 times higher odds), Black (1.30 times higher odds), American Indian/Alaska Native (1.19 times higher odds), and Multiracial (1.21 times higher odds) groups compared to White adults in 2022 2 (CDC.gov).
These disparities highlight the complex interplay of societal, economic, and cultural factors that contribute to stress levels across different demographic groups in the U.S.
Medical impact of chronic stress on Americans
Stress doesn’t just impact your mind; it affects your body, too. Chronic stress is now linked to a range of health conditions that place a strain on individuals and the healthcare system.
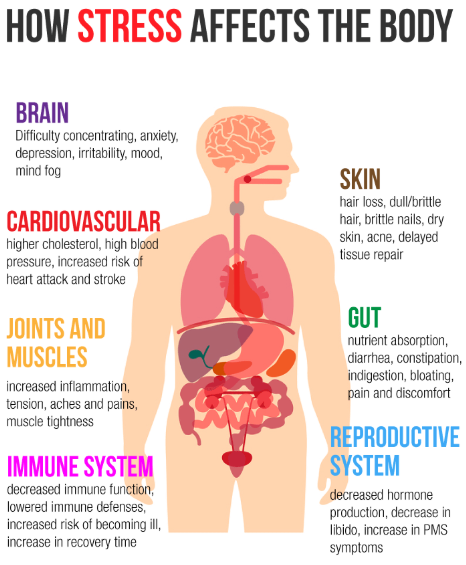
General impact and chronic illnesses
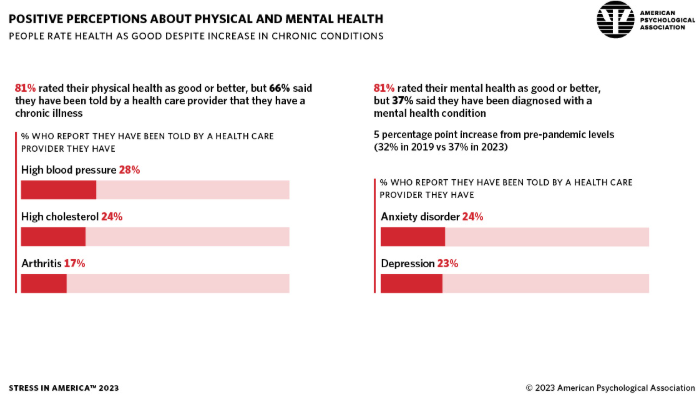
- Increased chronic illnesses: The long-term stress sustained since the COVID-19 pandemic began has significantly impacted well-being, evidenced by an increase in chronic illnesses (American Psychological Association).
- For adults aged 35-44, chronic illness diagnoses increased from 48% in 2019 to 58% in 2023.
- Two-thirds of adults (66%) reported in 2023 that they have been told by a healthcare provider they have a chronic illness, including high blood pressure (28%), high cholesterol (24%), or arthritis (17%).
- Physical symptoms of stress: Many Americans report experiencing physical symptoms related to stress (American Psychological Association).
- 77% experienced physical symptoms in the last month. Common symptoms include fatigue (51%), headache (44%), upset stomach (34%), and muscle tension (30%).
- Stress affects one’s health are independently associated with an increased likelihood of worse health and mental health outcomes.
- Individuals who reported a lot of stress and that stress impacted their health a lot had a 43% increased risk of premature death (National Library of Medicine).
Cardiovascular health
Chronic stress is a significant risk factor for heart disease, the leading cause of death in the United States.
- A study in The Lancet showed that people who reported high stress, a history of depression, and other psychosocial factors were 2.5 times more likely to have a heart attack than those with low stress or no history of depression (Yale Medicine).
Immune system dysfunction
Chronic stress can suppress and dysregulate the immune system, making individuals more susceptible to infections and inflammatory diseases.
- Impaired immune response: Chronic stress can interfere with the immune system’s normal function, including its ability to respond to anti-inflammatory signals.
- This may increase susceptibility to inflammatory diseases such as allergic, autoimmune, or cardiovascular diseases (American Psychological Association).
- Autoimmune diseases: Stress may both trigger and exacerbate autoimmune diseases.
- Up to 80% of patients have reported uncommon emotional stress before the onset of autoimmune diseases like rheumatoid arthritis, multiple sclerosis, inflammatory bowel disease (Crohn’s disease and ulcerative colitis), systemic lupus erythematosus, and Graves’ disease (Global Autoimmune Institute).
Digestive problems
The brain-gut connection is strong, and chronic stress significantly impacts digestive health.
- Gastrointestinal issues: Short-term stress can cause issues like diarrhea or vomiting, while long-term stress can lead to more chronic conditions (National Library of Medicine).
- Irritable Bowel Syndrome (IBS) is a common condition exacerbated by stress, and it’s twice as common in women as in men. Stress can worsen IBS symptoms like gas and bloating.
- Functional dyspepsia (chronic indigestion) and Irritable Bowel Syndrome were significantly more prevalent in groups with high stress compared to reference groups in a study on emotional stress and digestive diseases.
- Functional dyspepsia: 48.2% in high stress group vs. 29.4% in reference group.
- Irritable bowel syndrome: 46.5% in high stress group vs. 24.7% in reference group.
Mental health conditions
Chronic stress is intricately linked to mental health disorders, often acting as a trigger or exacerbating existing conditions.
- Increased mental health diagnoses (American Psychological Association):
- Adults ages 35-44 experienced the highest increase in mental health diagnoses, from 31% in 2019 to 45% in 2023.
- Adults ages 18-34 still reported the highest rate at 50% in 2023.
- More than one-third of adults (37%) said they have a diagnosed mental health condition in 2023, a 5 percentage point increase from pre-pandemic levels (32% in 2019). Most cited anxiety disorder (24%) or depression (23%).
Economic impact how much stress is costing the U.S
Stress is not just a personal issue; it’s an economic one, too. Here’s what the costs look like today. The medical impact of chronic stress also translates into enormous financial costs for the U.S. healthcare system and economy.
- Lost productivity and absenteeism:
- An estimated 1 million workers are absent every day due to stress (Center for Workplace Mental Health).
- Job stress is estimated to cost U.S. industries more than $300 billion annually in absenteeism, reduced productivity, and accidents (American Institute of Stress).
- Employees lose over five work hours each week due to stress-related thoughts and concerns (Center for Workplace Mental Health).
- Overall healthcare costs:
- Work-related stress alone contributes to $190 billion in annual healthcare costs in the United States (Cigna Healthcare).
- Estimates suggest that between 4% and 19% of health expenditure is attributable to stress-related illness, amounting to between US$717 million and US$133.2 billion annually (Cigna Healthcare).
- As much as 25% of hospital admissions, 35% of emergency department attendances, 19% of primary care visits, and 12% of outpatient attendances are likely the result of stress-related illness (Cigna Healthcare).
The data clearly demonstrates that chronic stress is not merely a feeling but a significant public health issue with severe medical ramifications and substantial economic consequences for the United States.
How are Americans coping?
Americans are employing a diverse range of strategies to cope with stress, with varying levels of effectiveness and notable generational differences in approach.
While there’s a growing openness to mental health discussions, many still struggle to manage their stress effectively and access necessary support.
General coping strategies and challenges
- Self-care practices are common, but often insufficient: Many Americans engage in widely recognized self-care, yet it doesn’t always fully mitigate pervasive stress (Civicscience.com).
- Common strategies include listening to music, spending time with friends/family, exercising, getting enough sleep, and eating healthy. (Mayo Clinic)
- However, only 28% of Americans report managing their stress “extremely well.” (American Psychological Association)
- Emotional support gap: Two-thirds of adults (66%) said they could have used more emotional support in the last 12 months, with 26% needing “a lot more” support. More than half (52%) wish they had someone for advice or support. (American Psychological Association)
- Reluctance to burden others: Around three in five adults (62%) avoid discussing their stress to avoid burdening others.(American Psychological Association)
- Financial stress silence: Only 52% of adults are comfortable discussing money/finances, and 45% feel embarrassed about their financial situation, despite finances being a top stressor. (American Psychological Association)
- Feeling overwhelmed/lost: 36% of adults don’t know where to start with stress management, and 33% feel completely stressed out regardless of their efforts. (American Psychological Association)
- Understating stress: Around two-thirds of adults (67%) downplay their stress, believing their problems aren’t “bad enough” compared to others. (American Psychological Association)
Therapy use
- Growing acceptance, persistent barriers: There’s increasing openness to mental health discussions, especially among younger generations, but significant hurdles remain for many in accessing therapy.
- Nearly one-quarter of Americans currently see a therapist. (Thriveworks 2025 Pulse on Mental Health Report)
- Almost half (48%) plan to start therapy within the next year, a 5% increase from the previous year. (Thriveworks 2025 Pulse on Mental Health Report)
- Top reasons for seeking therapy include anxiety and depression (over half of respondents), followed by stress and burnout (33%), trauma (27%), and relationship issues (25%). (Fierce Healthcare)
- Effectiveness: 78% of those who sought therapy reported seeing improvement. (Fierce Healthcare)
- Telehealth preference: Nearly a quarter of respondents prefer telehealth over in-person therapy. (Fierce Healthcare)
- Trends in psychotherapy: From 2018 to 2021, there was an increase in the use of only psychotherapy among adults receiving outpatient mental health care (from 11.5% to 15.4%). Psychotherapy visits per patient also increased. (National Library of Medicine)
- Barriers to Therapy:
- Cost is the leading barrier for Gen Z (43%). (Thriveworks 2025 Pulse on Mental Health Report)
- “Necessity” is the top reason cited by Millennials, Gen X, and Baby Boomers for avoiding therapy (e.g., 75% of Baby Boomers didn’t feel it was necessary). (Thriveworks 2025 Pulse on Mental Health Report)
- Other cited reasons for not seeking treatment include the belief that therapy doesn’t work (40%), lack of time (39%), and lack of insurance (37%). (American Psychological Association)
Exercise and physical activity
- Recognized stress reliever, mixed participation: Exercise is widely known for its stress-reducing benefits (releasing endorphins), but it’s no surprise that we don’t like to do it.
- 22% of adults use exercise or play sports as a common stress management activity. (The American Institute of Stress)
- Only 48.8% of U.S adults meet the minimum level of physical activity for good health. (National Library of Medicine)
Mindfulness and relaxation techniques
- Growing adoption: Practices like meditation and deep breathing are increasingly popular for stress management.
- The percentage of U.S. adults who practiced meditation more than doubled between 2002 and 2022, from 7.5% to 17.3%. (National Center for Complementary and Integrative Health)
- Mindfulness and expressive coping approaches are favored by Generation Z. (International Journal for Multidisciplinary Research)
Prescription medication
- Significant use, particularly for depression/anxiety:
- The rise in diagnosed mental health conditions (37% of adults now have a diagnosed condition, up from 32% pre-pandemic, with anxiety at 24% and depression at 23%) suggests a corresponding need for and potential increase in medication use for these conditions. (American Psychological Association)
Other noteworthy tools and tactics
- Social connection:
- Younger adults (18-34) prioritize social connection for mental health more than older adults (50+). (American Psychiatric Association)
- Gen Z favors social support as a coping approach.(International Journal for Multidisciplinary Research)
- Hobbies and self-care: Devoting more time to hobbies is a top five personal strategy for improving mental health among Millennials and Gen Z. Prioritizing self-care and eating healthier are also key. (Thriving Center of Psychology)
- Journaling: Keeping a stress journal is recommended to identify stressors and coping patterns. (HelpGuide.org)
- Unhealthy coping:
- Around 30% of U.S adults eat comfort food “more than usual” when stressed. (The American Institute of Stress)
- Substance abuse (alcohol, nicotine) is also a concern, though often temporary relief. (Healthline)
Generational differences in coping
- Gen Z & millennials (younger adults):
- Higher therapy engagement (and intent): While Gen Z may show some skepticism towards therapy (37% viewing it as “mentally weak”), they are still more likely to be in therapy or planning to go (nearly 1 in 5 currently in therapy, 39% planning in 2024). (Thriving Center of Psychology)
- Cost as a barrier: Cost is the leading barrier to therapy for Gen Z (43%). (Thriveworks 2025 Pulse on Mental Health Report)
- Openness to discussion: Generally more open about mental health, with 83% of Gen Z and Millennials in therapy openly sharing their status. (Thriveworks 2025 Pulse on Mental Health Report)
- Social media: Used for coping, but also a source of stress and potential misinformation. (Pew Research Center)
- Difficulty with boundaries: Gen Z (64%) and Millennials (59%) are more likely to have trouble saying “no” compared to older generations. (Thriveworks 2025 Pulse on Mental Health Report)
- Generation X:
- Tend to rely more on problem-solving and pragmatic coping strategies. (International Journal for Multidisciplinary Research)
- Often display autonomy and emotional restraint, preferring to manage challenges independently. (International Journal for Multidisciplinary Research)
- Baby boomers and older adults:
- Least likely to seek therapy: 80% of Baby Boomers state they would not seek mental health services, often citing lack of necessity. (Thriveworks 2025 Pulse on Mental Health Report)
- More likely to push through stress rather than seeking formal help. (SingleCare)
- Older adults may face greater difficulties accessing care, with over half aged 65+ not having had treatment in over five years. (Fierce Healthcare)
Stress demands our attention
Stress in 2025 isn’t slowing down, and its effects ripple across our health, economy, and communities. American workers, families, and businesses are increasingly aware of the stakes, but there’s clearly more work to be done to provide resources and reduce unnecessary burdens.
If you are experiencing a medical emergency, contact your medical provider or 911.
For media inquiries or commentary, please contact us.